C.M. is a 71-year-old patient with worsening GERD related symptoms of 30-year duration. After years of proton pump inhibitor therapy, she has stopped responding to medical treatment and decided to seek more effective GERD treatment options. An upper endoscopy with ambulatory pH testing showed a hiatal hernia and confirmed the diagnosis of GERD. Esophageal manometry revealed a hypercontractile esophagus without esophageal outflow obstruction. Of note, patient reported a history of dysphagia to solid food like rice and bread. She underwent esophageal balloon dilation around 5 years prior to presentation and her dysphagia related symptoms resolved. She also has primary hypertension and is on several anti-hypertensive medications including calcium channel blockers. She has no chest pain and her main complaint upon presentation was heartburn with occasional food regurgitation.
She was offered hiatal hernia repair with Nissen fundoplication. Patient agreed to proceed and underwent the procedure with no complications. Her GERD related symptoms immediately resolved. Two months after surgery she was tolerating regular diet with no dysphagia, regurgitation, or chest pain.
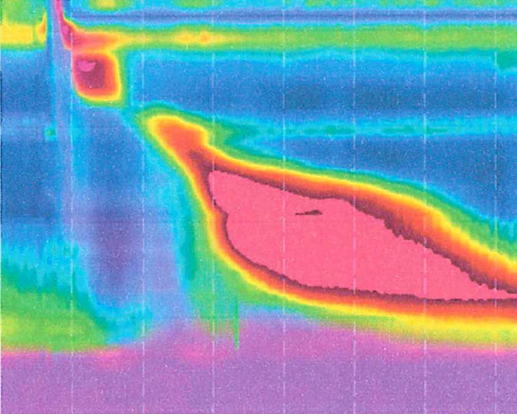
The incidence of hypercontractile esophagus (also called nutcracker esophagus) in GERD patients presenting for hiatal hernia repair and Nissen fundoplication is low. The presence of hypertensive esophageal contractions and normal peristalsis is, however, not a contraindication for Nissen fundoplication. The success rate of Nissen fundoplication in cases of hypertensive esophageal contractions remains high even in the presence of elevated lower esophageal sphincter resting pressure. It should be noted that diffuse esophageal spasm is different from hypercontractile esophagus and is characterized by uncoordinated and simultaneous contractions. Patients with diffuse esophageal spasm typically present with chest pain and around 20% of patients report heartburn. Calcium channel blockers, hydralazine and sublingual nitroglycerine are often used to relax the esophagus and alleviate symptoms. In certain cases, a long myotomy with partial fundoplication may be offered especially when patients do not respond to medications. Due to poor esophageal motility, Nissen fundoplication has been traditionally contraindicated in these cases.
Last, I would like to mention that there may be a causal relationship between esophageal motility disorder and GERD. Pelligrini et al report in the study I reference at the end of this blog that elevated contraction amplitude in nutcracker esophagus cases decreased after Nissen fundoplication. Whether GERD contributes to altered esophageal motility patterns remains to be determined.
Reference:
Outcomes of laparoscopic Nissen fundoplication in patients with the “hypercontractile esophagus”. Barreca M , Oelschlager BK, Pellegrini CA.
Arch Surg. 2002 Jun;137(6):724-8, discussion 729.