The patient is a 30 year-old female with symptomatic acid reflux in the setting of Schatzki’s ring and hiatal hernia. The ring was previously successfully dilated for dysphagia. However, heartburn and food regurgitation especially at night persisted due to the associated hiatal hernia. Esophageal manometry showed normal peristalsis and contractile wave amplitude. Accordingly, the patient was offered a hiatal hernia repair and Nissen fundoplication as the most reliable cure for her GERD related symptoms.
Intra-operatively, an enlarged caudate lobe was noticed after opening the gastro-hepatic ligament at the level of the pars-flaccida. The caudate lobe occupied most of the lesser sac and was abutting the spleen. The left gastric artery was prominent and a dilated branch emanating from the left gastric artery coursed toward the mediastinum between the right crus and esophagus. The spleen was slightly enlarged too and after taking down some of the short gastric blood vessels along the greater curvature, we noted massively dilated splenic hilum blood vessels. The posterior gastric artery was also dilated and several other tortuous blood vessels coursing along the left crus and entering the mediastinum were also noted. The liver surface was smooth with no apparent evidence of cirrhosis.
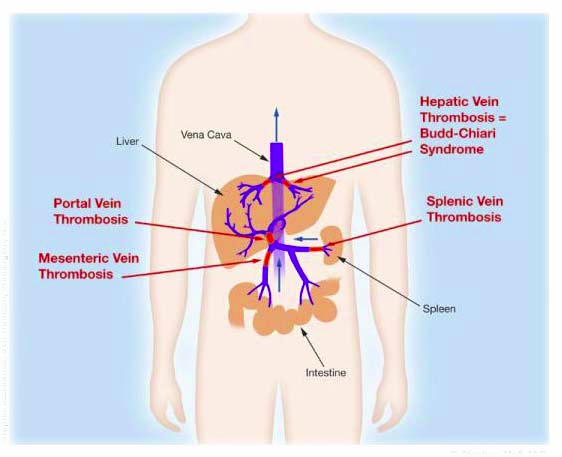
All these findings were suggestive of compensated portal hypertension in the setting of normal liver enzymes and normal looking liver surface suggestive of Budd-Chiari syndrome. Budd-Chiari is a rare syndrome affecting 1.4 per million people. It is characterized by hepatic venous outflow obstruction and is asymptomatic in 20% of the patients. Myeloproliferative disorders must be ruled out and long-term treatment depends on chronic anticoagulation and close follow ups. Patients who fail anti-coagulation require more aggressive interventions like porto-systemic shunting and liver transplantation.
I thought this was an interesting case to share. I have never encountered such findings in a completely asymptomatic patient. Do no harm is a guiding principle in my practice. Taking down these blood vessel collaterals to dissect the hiatal hernia would have led to liver decompensation and serious injury. This is one of the few GERD cases where I think long-term Nexium or Prilosec is definitely much safer than Nissen fundoplication surgery.