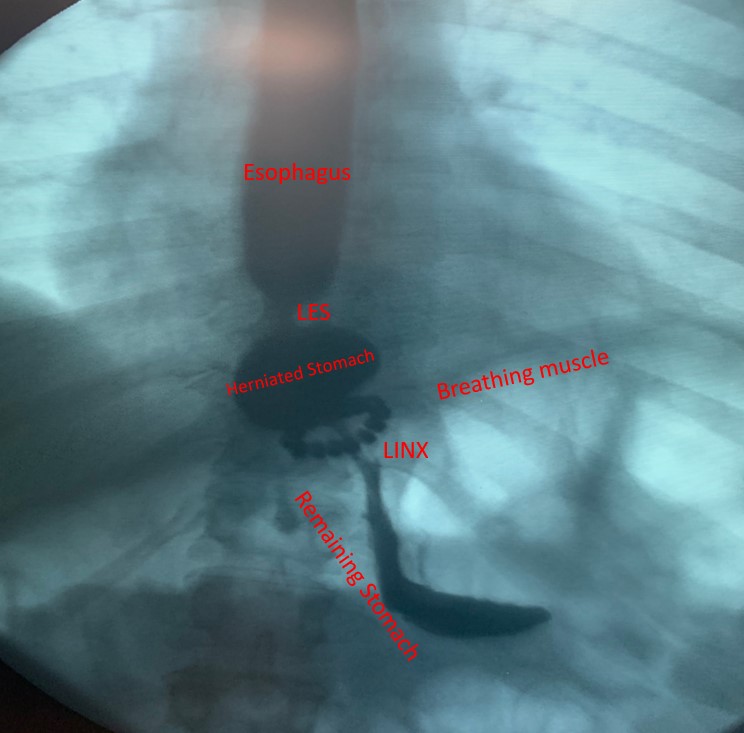
LINX™ Reflux Management system consists of a bracelet of magnetic beads that is placed around the esophagus to reinforce the weakened lower esophageal sphincter. LINX™ or magnetic sphincter augmentation procedure is done under general anesthesia using the same approach as a laparoscopic Nissen fundoplication.
During swallowing, as food passes through the esophagus, LINX™ magnetic beads separate allowing the food bolus to pass into stomach and then close preventing acid reflux.
In 2012 the FDA approved LINX™ procedure for GERD treatment based on a prospective study that was published in the New England Journal of Medicine. 100 patients with increased esophageal acid exposure underwent the procedure. At one year follow up, 58% of patients had normal esophageal acid exposure. The most frequent adverse event was dysphagia (difficulty swallowing), which occurred in 68% of patients.
Subsequent follow up of this patient cohort at 5 years after LINX™ implantation showed:
12% persistent heartburn
1% persistent food regurgitation
15% dependency on proton pump inhibitors
6% difficulty swallowing
7% LINX™ device removal
At Houston Heartburn and Reflux Center, Dr Darido does not offer magnetic sphincter augmentation or LINX™ surgery. Dr Darido offers hiatal hernia repair and Nissen fundoplication, the gold standard treatment for acid reflux disease. However, if you had magnetic sphincter augmentation or LINX™ surgery and you continue to struggle with heartburn, food regurgitation, chest pain or difficulty swallowing we can help you.
Is LINX™ revision surgery appropriate for you?
At Houston Heartburn and Reflux Center, each patient receives a thorough evaluation for heartburn and acid reflux. Depending on your symptoms and work up findings, LINX™ device removal and conversion to Nissen or Toupet fundoplication may be indicated. Please request an appointment to see if LINX™ revision surgery is appropriate for you.